Mechanical (or forced) ventilators are often used by physicians when a patient is incapable of maintaining spontaneous ventilation (breathing). It is used in acute settings such as in the Intensive Care Unit (ICU) when a (endotracheal) tube is inserted into the patient’s airway to force air inside the lungs. Mechanical ventilation is often a life-saving intervention, but carries many potential complications including ventilator-induced lung injury, alveolar damage, ventilator-associated pneumonia and pneumothorax (i.e. accidental presence of air/gas in pleural cavity). Even today, there remain significant challenges in developing strategies (or sequences) to optimize management of ventilator-dependent patients. To this regard, we are investgating two areas of pulmonary flow under mechanical ventilation conditions
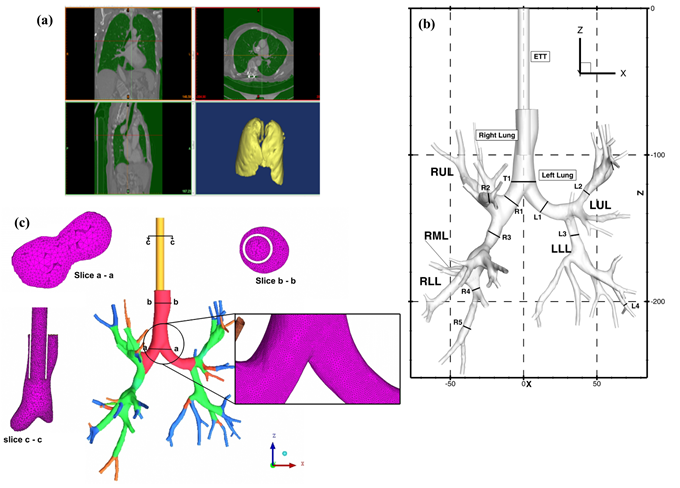
- Large Eddy Simulation for targeted nanoparticle drug delivery and reduction of ventilator mediated injuries in human lungs: CFD models of air-flow and particle deposition in the extrathoracic passages could be of great use in the development of aerosol based therapies. The airflow patterns through these extrathoracic passages affect the trajectories of entrained particles and must be understood in order to determine drug dosimetry patterns among the distal (i.e. downstream) thoracic airways. The airflow patterns are governed by the morphologies of the respective nasal, oral, pharyngeal, and laryngeal airways in association with ventilatory variables. The advantage of using three-dimensional CFD models compared to in vitro studies is that the modelling results can readily determine localized deposition characteristics.
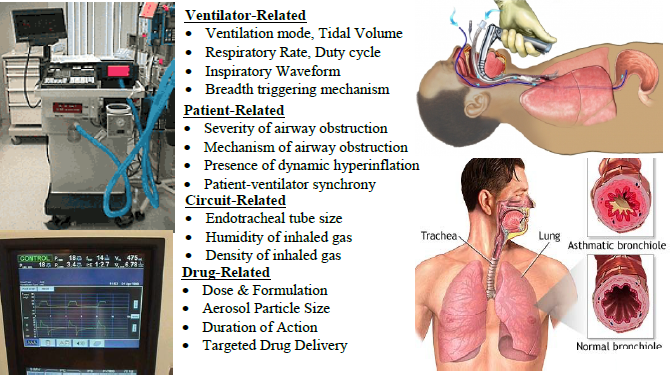
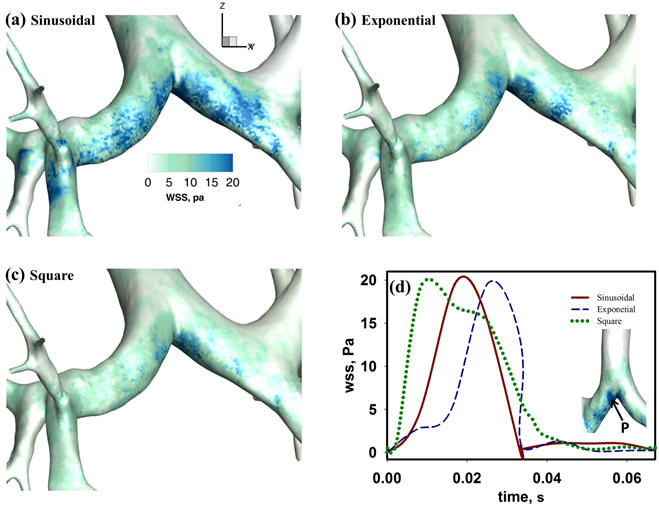
- Pulmonary Therapy using High Frequency Oscillatory Ventilation: Mechanical ventilation is often used by clinician as a supportive therapy to patients who are unable to maintain adequate gas exchange. Invasive high frequency oscillatory ventilation (HFOV) is an alternative form of mechanical ventilation mode that is employed when conventional mechanical ventilation (CMV) fails to provide appropriate oxygenation or carbon dioxide elimination; or, in critical situations, where usage of CMV based therapy also leads to lung injury. The rationale for the use of HFOV is its ability to provide adequate ventilation while at the same time protecting the patient lung from injury. This is achieved by delivering a shallow tidal volume (~1-2 ml/kg) at high frequencies (1-30 Hz) during each cycle. Pulmonary flow physics based on this strategy of ventilation management is very complex and is not yet fully understood as opposed to CMVwhere bulk convection is considered to be the main mechanism of flow transport .Computational studies of fluid flow during HFOV has identified several additional physical mechanisms that may play an important role in gas transport and mixing in additional to the bulk convection mechanism which dominates CMV. These additional mechanisms are: (a) asynchronous gas exchange between respiratory units (also defined as Pendelluft); (b) bidirectional counter flow; (c) longitudinal mixing; and, (d) gas exchange by molecular diffusion. Majority of this earlier reported work are limited in scope and do not fully take into account various (ventilator) device specific conditions that are vital to critical care clinicians. Our aim is to bridge this gap and understand HFOV fluid dynamics for clinically relevant conditions.

- Sponsors: Current: Lehigh University Start-up Funds; Past: University of Missouri Research Board (seed grant)
- Collaborators: Gary A Salzman (UMKC)
- Current Students: Rahul R Rajendran (PhD-Lehigh)
- Former Students: Mohammed Alzahrany (PhD-Lehigh); Timothy Van Rhein (MS-Missouri S&T)
Publications (most recent first):
- Investigation of mucus transport in an idealized lung airway model using multiphase CFD analysis - Rahul Rajendran and Arindam Banerjee, APS-DFD2015, Boston, MA.
- Fluid flow and particle transport in mechanically ventilated airways. Part I: Fluid flow structures, Medical & Bilogical Engineering & Computing, Timothy Van Rhein, Mohammed Alzahrany, Arindam Banerjee and Gary Salzman (2015).
- Fluid flow and particle transport in mechanically ventilated airways. Part II: Particle transport, Medical & Bilogical Engineering & Computing, Mohammed Alzahrany, Timothy Van Rhein, Arindam Banerjee and Gary Salzman (2015).
- Role of carrrier gases in enhancement of gas exchange and aerosol-drug delivery under invasive high frequency oscillatory ventilation, Mohammed Alzahrany and Arindam Banerjee, Journal of Aerosol Science, 88 : 1-18 (2015).
- A biomechanical model of pendelluft induced lung injury, Mohammed Alzahrany and Arindam Banerjee, Journal of Biomechanics, 48 (10): 1804-1810 (2015)
- Aerosolized drug delivery in patient-specific lung model during invasive high frequency oscillatory ventilation, Mohammed Alzahrany and Arindam Banerjee, Journal of Aerosol Science, 81 (3): 1-20 (2015).
- The role of coupled resistance-compliance in upper tracheobronchial airways under high frequency oscillatory ventilation - Mohammed Alzahrany, Arindam Banerjee and Gary Salzman, Medical Engineering and Physics, 36 (12): 1593-1604 (2014).
- Flow transport and gas mixing during invasive high frequency oscillatory ventilation - Mohammed Alzahrany, Arindam Banerjee and Gary Salzman, Medical Engineering and Physics, 36 (6): 647-658(2014).
- Effect of time-dependent pressure boundary conditions on flow transport in a patient specific lung model during invasive high frequency oscillatory ventilation - Mohammed Alzahrany and Arindam Banerjee, APS-DFD2013, Pittsburgh, PA.
- Numerical investigation of pulmonary drug delivery under mechanical ventilation conditions- Arindam Banerjee & Tim Vanrhein - APS-DFD2012, San Diego, California.
- Effects of pressure controlled waveforms on flow transport and gas mixing in patient specific lung model during invasive HFOV - Mohammed Alzahrany & Arindam Banerjee - APS-DFD2012, San Diego, California.
- Numerical investigation of aerosolized drug delivery in the human lungs under mechanical ventilator conditions – Tim Vanrhein and Arindam Banerjee –APS-DFD2010, Nov. 22-24, Long Beach, California.
